Call Today (210) 796-8077
ARVCenters is Giving Away 50 FREE Frozen Shoulder Consultation Vouchers for a limited time!
For the Next Week, we are giving away 50 FREE Vouchers for a
Frozen Shoulder Pain Assessment, a Detailed Orthopedic Examination, a Review of your Past Medical History, an Imaging Review AND a Personalized Treatment Plan (If you Qualify), all for FREE! (Normally a $345 Total Value)
Watch a Demonstration and Explanation of a Revolutionary Treatment for Frozen Shoulder Syndrome (Adhesive Capsulitis)
Are you suffering from...
Persistent Shoulder Pain?
Loss of Movement?
Diagnosed with Frozen Shoulder Syndrome?
Diagnosed with Adhesive Capsulitis?
Failed Physical Therapy?
Failed Steroid Injections?
Failed AIRROSTI?
The Hidden Cause of Persistent Shoulder Pain:
Beyond the Joint Capsule

Frozen shoulder, or adhesive capsulitis, is more than just a stiff joint. It’s a complex inflammatory condition driven by a process called neovascularization—the formation of abnormal new blood vessels. These vessels create a vicious cycle of inflammation and pain that conventional treatments simply can’t break.
“The underlying pathology of Adhesive Capsulitis is the combination of synovial inflammation and capsular fibrosis.” - Liang et al. [1]
While your doctor may have explained that your joint capsule is inflamed and thickened, they may not have discussed the critical role these abnormal blood vessels play in perpetuating your pain. This is the missing piece of the puzzle that explains why your previous treatments have failed to provide lasting relief.
Why Conventional Treatments Fall Short
Conventional treatments for frozen shoulder are designed to manage symptoms, not to address the root cause of the problem. Here’s a breakdown of why these common approaches often fail to deliver long-term results:
Physical Therapy and Range-of-Motion Exercises focus on stretching the shoulder capsule to improve mobility, but they cannot eliminate the underlying inflammation or the abnormal blood vessels that perpetuate your pain. While you may experience temporary improvement during therapy sessions, the inflammatory process continues unchecked, causing symptoms to return.
Steroid Injections provide temporary anti-inflammatory effects by reducing swelling in the joint. However, research reveals a sobering reality: nearly 30% of patients experience treatment failure with intraarticular corticosteroid injections, requiring additional interventions or progression to surgical management within 12 months [2]. The effects are temporary because the injections don't address the neovascularization that drives the inflammatory cycle.
Pain Medications including NSAIDs, prescription painkillers, and anti-inflammatory drugs only mask the pain signals sent to your brain. While they may provide temporary symptom relief, they do nothing to resolve the underlying pathological process. You're essentially putting a band-aid on a problem that requires surgical precision to fix.
Manipulation Under Anesthesia and Surgery represent the most aggressive conventional approaches, but even these invasive procedures carry significant risks and may not address the vascular component of the disease. Studies show that even after "successful" conventional treatment, approximately 40-50% of patients experience persistent symptoms, and many retain some degree of pain and stiffness even years later.
The fundamental problem with all conventional treatments is that they are fighting a losing battle against the persistent inflammation and neovascularization that are the true culprits behind your chronic pain. Until these abnormal blood vessels are eliminated, the cycle of inflammation and pain will continue, regardless of how many treatments you try.
How Shoulder Joint Embolization Works
Shoulder joint embolization is a non-surgical procedure performed by an interventional radiologist. Here’s how it works:
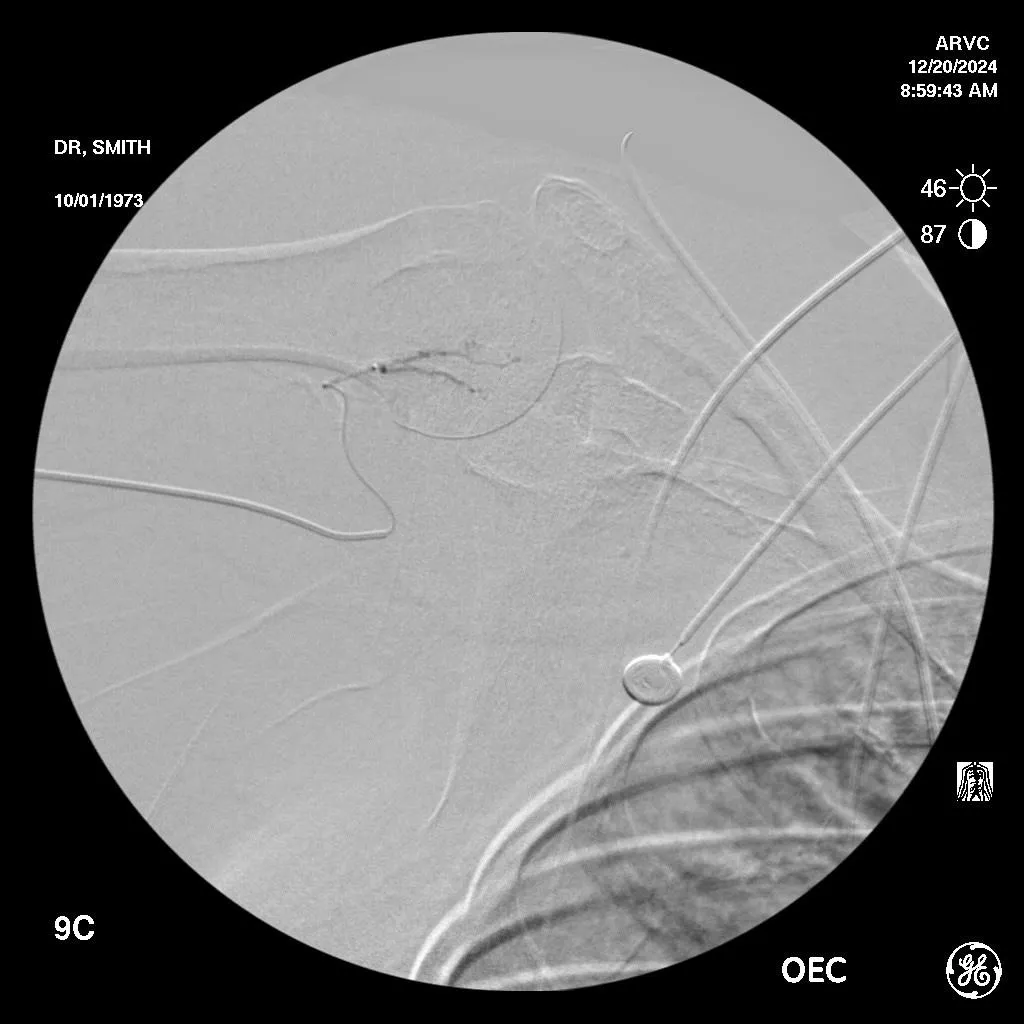
1. Mapping the Abnormal Vessels: Using advanced imaging, the interventional radiologist identifies the specific abnormal blood vessels that are feeding the inflammation in your shoulder.
2. Blocking the Blood Flow: Tiny, microscopic particles are injected into these abnormal vessels, blocking the blood flow that fuels the inflammation.
*(This does not disrupt blood flow to the normal healthy tissue)
3. Breaking the Cycle of Pain: By restricting blood flow to the inflamed tissue, the procedure breaks the cycle of inflammation and pain, allowing your shoulder to heal naturally.
The Evidence: Real Results for Patients Like You
The clinical evidence for shoulder joint embolization is compelling. Studies have shown that patients who undergo this procedure experience:
• Significant Pain Reduction: Patients report a dramatic decrease in pain within weeks of the procedure.
• Improved Range of Motion: With the inflammation resolved, patients regain mobility and function in their shoulder.
• Lasting Relief: Because the procedure addresses the root cause of the pain, the results are long-lasting.
In a recent study, patients who underwent shoulder joint embolization experienced significant reductions in pain and improvements in function at 1, 3, and 6 months after the procedure [1].
Before Embolization
Shaded areas around vessels are called "hyperemia" and are the abnormal growth of micro blood vessels causing pain and inflammation.
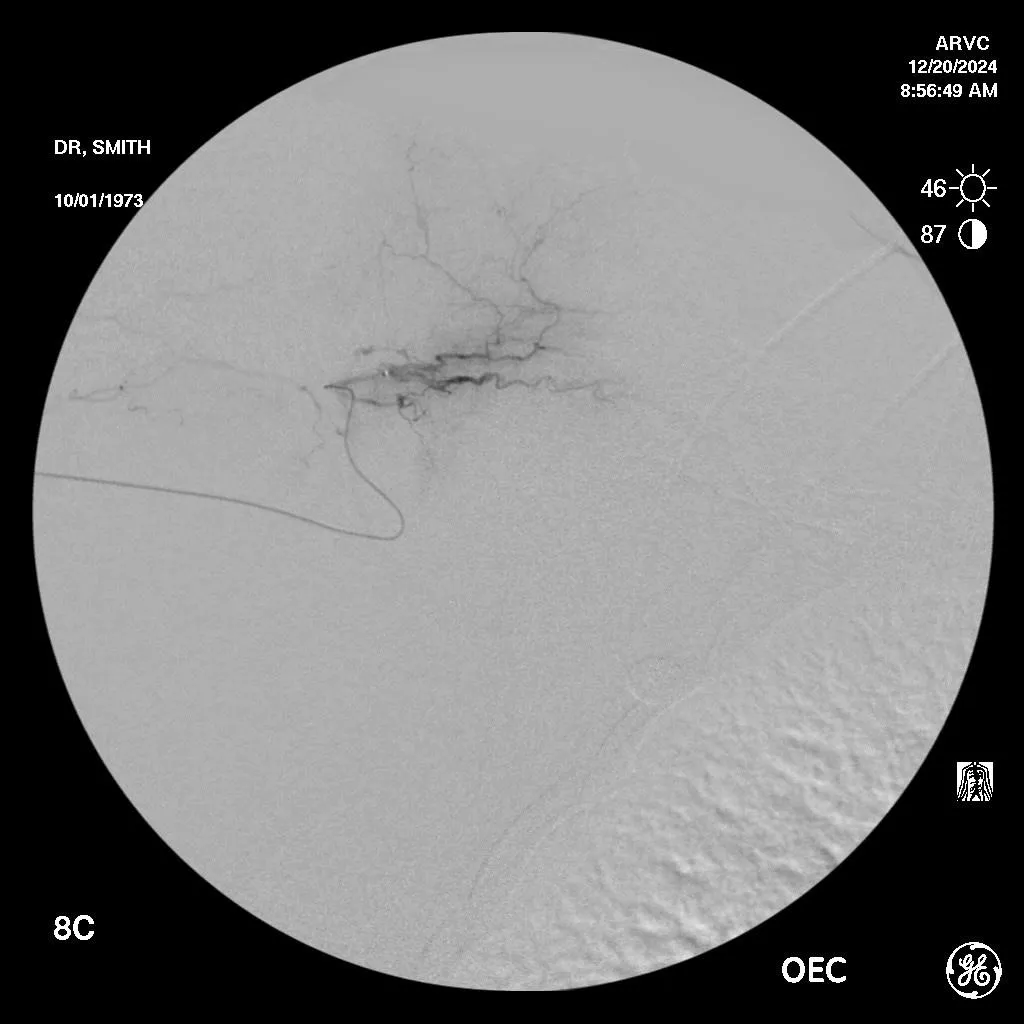
After Embolization
After embolization, the excessive hypervascularization "disappears" improving pain and function by eliminating the source of the inflammation.
References
[1] Liang, K. W., Lin, H. Y., Hsu, K. L., Kuan, F. C., Gean, C. Y., Wang, C. K., ... & Wang, B. (2025). Clinical and Radiological Outcomes of Transarterial Embolization for Adhesive Capsulitis. Korean Journal of Radiology, 26(3), 230–238. https://pmc.ncbi.nlm.nih.gov/articles/PMC11865901/
[2] Hanish, S. J., Resnick, M. L., Kim, H. M., & Smith, M. J. (2022). Predictive Factors for Failure of Intraarticular Injection in Management of Adhesive Capsulitis of the Shoulder. Journal of Clinical Medicine, 11(20), 6212. https://pmc.ncbi.nlm.nih.gov/articles/PMC9605176/
Meet Our Interventional Radiologists
Preston G. Smith, M.D
Dr. Preston George Smith is a Board Certified Vascular & Interventional Radiologist. Following his graduation from the University of Texas Medical School in the Texas Medical Center in Houston he completed his Radiology Residency at Rush University Medical Center in Chicago.
Board Certified Vascular & Interventional Radiology

Arthur S. Joseph, D.O.
Dr. Joseph is an accomplished Interventional Radiologist with a passion for delivering minimally invasive, image-guided procedures to improve patient outcomes. He is Board-Certified in Diagnostic and Interventional Radiology by the American Board of Radiology.
Board Certified Vascular & Interventional Radiology

Samy A. Al-Bayati, M.D.
Dr. Samy Al-Bayati is an accomplished physician with extensive experience in both Urology and Interventional Radiology. He currently serves as a faculty member at the University of Texas Health Science Center in San Antonio, Texas.
Board Certified Vascular & Interventional Radiology

Ahmed A. Farag, M.D.
Ahmed A. Farag, M.D. is a Board Certified Vascular & Interventional Radiologist. Dr. Farag grew up in Kentucky and attended the University of Louisville where he completed his Master’s Degree in Electrical Engineering prior to attending medical school also at the University of Louisville.